Are there exceptions to the one-lesion criteria?
Yes, if a sporadic patient has been treated with radiation or has a developmental venous anomaly (DVA), they may have multiple lesions and still have a sporadic form. A DVA is essentially a large vein that, on its own, is of little clinical significance.
Research has shown that DVAs are often located very close to sporadic CCMs, while they are very rarely seen in cases of familial CCM. People with a DVA sometimes develop more than one lesion in the area of the DVA.
These individuals still have sporadic CCM and won’t pass the illness to their children. (In the extremely rare cases of individuals with hereditary CCM and a DVA, one would expect to see many other lesions, scattered throughout the brain.)
 How can I confirm I have sporadic CCM?
How can I confirm I have sporadic CCM?
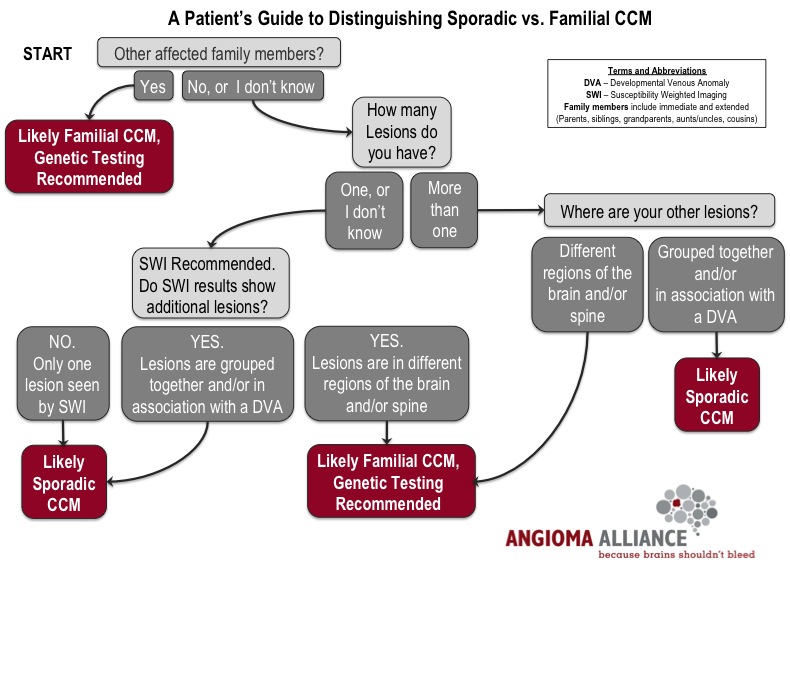
It is well known that sporadic CCM is not caused by genetic mutations that are inherited from one’s parent. Therefore, genetic testing of sporadic patients will not provide useful or beneficial information. However, even though genetic testing is not recommended for sporadic CCM patients, there is still something that you can do. You can work with your doctor to confirm your sporadic diagnosis using advanced imaging technology.
What is advanced imaging technology, and how can this be done?
Having a T2 weighted gradient echo (T2*GRE) MRI has been the long-time gold standard for identifying CCM lesions. However, there are more sensitive techniques, including susceptibility-weighted imaging (SWI), that have been shown to be ideal for detecting tiny, newly forming lesions in familial CCM.
Susceptibility-weighted imaging (SWI) is the best way to determine whether you have sporadic CCM because it allows you to rule out the presence of smaller lesions scattered throughout the brain typical of familial CCM. Having SWI will give you and your doctor the information to determine whether genetic testing may be advisable. Additionally, knowing that you have the sporadic form of the disease (solitary lesion using SWI MRI or a small number of lesions with an associated DVA) would free you from the worry that other family members could inherit the same disease.
How do sporadic lesions develop?
Recent evidence suggests that the cause of sporadic CCM lesion development is quite similar to familial CCM lesions. Researchers have found that there are genetic mutations of the CCM genes, but that these mutations occur only in the blood vessels of the sporadic CCM lesion. These mutations are not heritable; they are randomly acquired within brain blood vessels and cause a CCM lesion to form. Another vascular malformation, a developmental venous anomaly may set the stage for the formation of most sporadic lesions.
This data suggests that all forms of CCM lesions develop as the result of a similar mechanism (a complete loss of function of one of the CCM genes within the brain blood vessel cells). Because of this biological similarity, there is optimism that the same therapeutic drug may treat all forms of CCM in the future.
How do I fit into clinical drug trials and eventual treatments?
Another new discovery from the research front revealed that the same molecular disturbances causing the familial CCM are also present in the lesions themselves in sporadic cases. This means that treatments being developed for familial CCM may ultimately also target and benefit people with the sporadic form of the disease. But it remains critical to know whether your illness is truly sporadic or familial, for your own counseling, for your relatives, and for grouping the cases in appropriate clinical trials.
As we begin to focus more on clinical research, we will need everyone’s help.
A call to action
- Talk to your doctor to define your disease: do you have a DVA? Have you had SWI imaging?
- Join the Susan Sukalich Cavernous Malformation Patient Registry to be notified about upcoming studies for which you may qualify.
— Amy Akers, Ph.D. and Issam Awad, MD, MSc, FACS
References
-
Awad IA, et. al. cavernous malformations: deconstructing and neurosurgical disease. Ju Neurosurg. 2019 July 1;131(1):1-13.
-
McDonald DA, et. al. Lesions from patients with sporadic cerebral cavernous malformations harbor somatic mutations in the CCM genes: evidence for a common biochemical pathway for CCM pathogenesis. Hum Mol Genet. 2014 Aug 15;23(16):4357-70.
-
Spiegler S, et. al. High mutation detection rates in cerebral cavernous malformation upon stringent inclusion criteria: one-third of probands are minors. Mol Genet Genomic Med. 2014 Mar;2(2):176-85.
-
Petersen TA et. al. Familial versus sporadic cavernous malformations: differences in developmental venous anomaly association and lesion phenotype. AJNR Am J Neuroradiol. 2010 Feb;31(2):377-82.
-
de Champfleur NM et. al. Magnetic resonance imaging evaluation of cerebral cavernous malformations with susceptibility-weighted imaging. Neurosurgery. 2011 Mar;68(3):641-7; discussion 647-8.
Last updated 3.26.23


